Bursitis Of The Feet Treatment
Retrocalcaneal Bursitis is an inflammation of the protective sack between the heel bone and the Achilles tendon. It is the inflamed bursa that produces the redness and swelling associated with Haglund's deformity.
Causes
Feet are extremely resilient and are designed to stand up to the pressures of day-to-day living. In some cases, though, foot structures may break down when subjected to chronic stress associated with long periods of weight-bearing activity on concrete, asphalt, or other hard surfaces (especially when footwear does not allow for proper weight distribution). Foot problems, including infracalcaneal bursitis, are often made worse by poorly designed footwear, and pressure, impact, and shear forces can damage the feet over time. Bursal sacs are intended to minimize this damage, but sometimes the bursa itself becomes inflamed. A rapid increase in physical activity levels or thinning of the heel?s protective fat pad are factors that may contribute to infracalcaneal bursitis. Other possible causes of infracalcaneal bursitis include blunt force trauma. Arthritic conditions. Acute or chronic infection. The following factors may increase a person?s risk of bursitis, including infracalcaneal bursitis. Poor conditioning. Exposure to cold weather. Participating in contact sports. Having a previous history of bursitis in any joint. Heel striking when running, especially in conventional running shoes with heel elevation.
Symptoms
The following are the most common symptoms of bursitis. However, each individual may experience symptoms differently. Bursitis can cause pain, localized tenderness, and limited motion. Swelling and redness may occur if the inflamed bursa is close to the surface (superficial). Chronic bursitis may involve repeated attacks of pain, swelling, and tenderness, which may lead to the deterioration of muscles and a limited range of motion. The symptoms of bursitis may resemble other medical conditions or problems. Always consult your doctor for a diagnosis.
Diagnosis
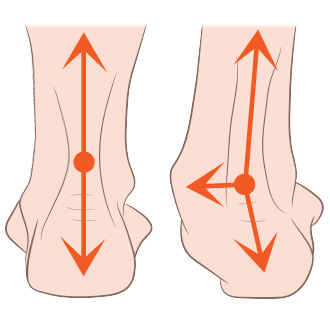
Your doctor will take a history to find out if you have the symptoms of retrocalcaneal bursitis. By examining your ankle, he or she can generally tell the location of the pain. The physician will look for tenderness and redness in the back of the heel. The pain may be worse when the doctor bends the ankle upward (dorsiflex), as this may tighten the achilles tendon over the inflamed bursa. Alternatively, the pain may be worse with toe rise, as this puts stress on the attachment of the achilles tendon to the heel bone. Imaging studies such as X-ray and MRI are not usually necessary at first. If initial treatment fails to improve the symptoms, these studies may be obtained. MRI may show inflammation.
Non Surgical Treatment
If you follow these steps, most attacks of bursitis should subside in four or five days and all symptoms should be gone within two weeks. Rest the body part that hurts. If you suspect that one activity has caused the pain, stop it until the pain is entirely gone. A sling, splint, or padding may be needed to protect the area from possible bumps or irritation. Try over-the-counter pain relievers. Nonprescription NSAIDs (aspirin, ibuprofen, and naproxen) will help reduce pain and swelling, though they won?t accelerate healing. Acetaminophen will help with pain but it doesn?t reduce inflammation. Ice it, then heat it. Apply ice packs during the first two days to bring down swelling. Then use heat-warm baths or a heating pad (on a medium or low setting)-to ease pain and stimulate blood flow. Don?t push it. Resume exercising only after you feel better. Start with gentle activity. Skip the liniments. Liniments and balms are no help for bursitis. Liniments don?t penetrate deeply enough to treat bursitis, they mainly warm the skin and make it tingle, thus distracting attention from the pain beneath. Massage is likely to make matters worse. Undergo physical therapy. Physical therapy strengthens joint muscles that have been affected by bursitis and may help prevent the bursitis from getting worse.
Surgical Treatment
Surgery is rarely need to treat most of these conditions. A patient with a soft tissue rheumatic syndrome may need surgery, however, if problems persist and other treatment methods do not help symptoms.
Treatment For Hammer Toes
 Overview
Overview
Generally a hammertoe or mallet toe is caused by wearing high heels or shoes that are too small around the toe area, so it?s no surprise that it is mostly women who suffer from them. A Hammer toes has a bend in the middle joint of the toe whereas a mallet toe has a bend in the upper joint of the affected toe. The way someone walks (gait) can also lead to the formation of hammertoes and mallet toes as can overuse and injury. Sometimes a deep blister will form over the bent joint and often after some time calluses and corns will develop on the affected toe joint. People with arthritis, diabetes or neuromuscular conditions are also more likely to develop a hammer toe or mallet toe.
Causes
Hammer toe most frequently results from wearing poorly fitting shoes that hammertoes can force the toe into a bent position, such as excessively high heels or shoes that are too short or narrow for the foot. Having the toes bent for long periods of time can cause the muscles in them to shorten, resulting in the hammer toe deformity. This is often found in conjunction with bunions or other foot problem (e.g., a bunion can force the big toe to turn inward and push the other toes). It can also be caused by muscle, nerve, or joint damage resulting from conditions such as osteoarthritis, rheumatoid arthritis, stroke, Charcot-Marie-Tooth disease, complex regional pain syndrome or diabetes. Hammer toe can also be found in Friedreich's ataxia.
 Symptoms
Symptoms
People with a hammer toe will often find that a corn or callus will develop on the top of the toe, where it rubs against the top of the footwear. This can be painful when pressure is applied or when anything rubs on it. The affected joint may also be painful and appear swollen.
Diagnosis
The exam may reveal a toe in which the near bone of the toe (proximal phalanx) is angled upward and the middle bone of the toe points in the opposite direction (plantar flexed). Toes may appear crooked or rotated. The involved joint may be painful when moved, or stiff. There may be areas of thickened skin (corns or calluses) on top of or between the toes, a callus may also be observed at the tip of the affected toe beneath the toenail. An attempt to passively correct the deformity will help elucidate the best treatment option as the examiner determines whether the toe is still flexible or not. It is advisable to assess palpable pulses, since their presence is associated with a good prognosis for healing after surgery. X-rays will demonstrate the contractures of the involved joints, as well as possible arthritic changes and bone enlargements (exostoses, spurs). X-rays of the involved foot are usually performed in a weight-bearing position.
Non Surgical Treatment
If your hammertoe problem is diagnosed as flexible hammertoe, there are a number of nonsurgical treatments that may be able to straighten out your toe or toes and return them to their proper alignment. Padding and Taping. Your physician may pad the boney top-part of your hammertoe as a means of relieving pain, and may tape your toes as a way to change their position, correct the muscle imbalance and relieve the pressure that led to the hammertoe's development. Medication. Anti-inflammatory drugs such as aspirin and ibuprofen can help deal with inflammation, swelling and pain caused by your hammertoe. Cortisone injections may be prescribed for the same purpose. If your hammertoe is a consequence of arthritis, your physician may prescribe medications for that.
Surgical Treatment
Toe Relocation procedures are ancillary procedures that are performed in conjunction with one of the two methods listed about (joint resection or joint mending). When the toe is deformed (buckled) at the ball of the foot, then this joint often needs to be re-positioned along with ligament releases/repair to get the toe straight. A temporary surgical rod is needed to hold the toe aligned while the ligaments mend.
 Prevention
Prevention
To help prevent hammer toes from developing, wear shoes or boots that provide sufficient width in the toe box to ensure minimal compression. Use inserts that help the toes flatten out and spread and give sufficient support to the metatarsal arch in the forefoot. If hammer toes have already formed, padded socks help protect the tops and the tips of the hammer toes and may reduce pain from rubbing and chafing.
What Can Cause Bunions?
Overview
 A bunion (Hallux Abducto Valgus) is sometimes described as a bump on the side of the big toe. However, the visible bump actually reflects changes in the bony framework in the front part of the foot. Instead of pointing straight ahead, the big toe leans towards the second toe, throwing the bones out of alignment and producing the ?bump? of the bunion. Bunions are a progressive disorder and gradually change the angle of the bones in your foot over the years. Symptoms usually occur in the later stages. The skin over the base of your big toe may become red and tender, and make wearing shoes painful. The bigger the bunion gets, the more it hurts to walk. Pressure from your big toe can force your second toe out of alignment, sometimes overlapping your third toe. Severe bunions can make it difficult to walk and you may develop arthritis.
A bunion (Hallux Abducto Valgus) is sometimes described as a bump on the side of the big toe. However, the visible bump actually reflects changes in the bony framework in the front part of the foot. Instead of pointing straight ahead, the big toe leans towards the second toe, throwing the bones out of alignment and producing the ?bump? of the bunion. Bunions are a progressive disorder and gradually change the angle of the bones in your foot over the years. Symptoms usually occur in the later stages. The skin over the base of your big toe may become red and tender, and make wearing shoes painful. The bigger the bunion gets, the more it hurts to walk. Pressure from your big toe can force your second toe out of alignment, sometimes overlapping your third toe. Severe bunions can make it difficult to walk and you may develop arthritis.
Causes
Bunions are among the most common problems of the foot. They are several possible reasons a bunion may develop, though a biomechanical abnormality (improper function of the foot) is the most common cause. In an unstable flat foot, for example, a muscular imbalance often develops that, over time, causes bunions. Bunions tend to run in families, and most podiatrists believe that genetic factors play a role in predisposing some people to develop bunions. Poor shoes, like high heels and pointed toe boxes--exacerbate the condition by speeding up the development of bunions, and by making bunions more painful. Poor shoe choices is at least one of the reasons bunions are much more common in women than men.
Symptoms
A bulging bump on the outside of the base of your big toe. Swelling, redness or soreness around your big toe joint aggravated by footwear. Red, calloused skin along the inside edge of the big toe. Corns or calluses under the ball of the foot or where the first and second toes overlap. Persistent or intermittent pain. Restricted movement of your big toe.
Diagnosis
Although bunions are usually obvious from the pain and unusual shape of the toe, further investigation is often advisable. Your doctor will usually send you for X-rays to determine the extent of the deformity. Blood tests may be advised to see if some type of arthritis could be causing the pain. Based on this evaluation, your doctor can determine whether you need orthopaedic shoes, medication, surgery or other treatment.
Non Surgical Treatment
A bunion treatment must address the underlying cause of the deformity, not just the bump (bunion) itself but also the functions of the foot. The up and down motion of the longitudinal arches in the foot. The sideways motion of the transverse arch. Bunion aids effectively treat this underlying foot function while straightening the big toe because the mid-foot strap stabilizes the longitudinal arches and transverse arch. The toe strap gradually and gently pulls the big toe away from the second toe. The metatarsal pad helps align the transverse arch. The hinged splint enables the big toe to flex while walking and adapts to the contour of the foot, especially around the inflamed area of the joint. 
Surgical Treatment
Your podiatrist can refer you to a podiatric surgeon who will evaluate the extent of the deformity. A podiatric surgeon can remove the bunion and realign the toe joint in an operation generally referred to as a bunionectomy. However, there are actually around 130 different operations that fall under this title, so don?t presume you?ll need the same type of surgery as that friend of a friend who couldn?t walk for 3 months.
Will Overpronation Need Surgical Treatments
Pronation is the term used to describe a natural movement of the foot when walking. When the gait is normal, the heel strikes the ground first. As weight is transferred forward, the arch of the foot flattens and the foot rolls slightly inwards. Body weight is then placed on the ball of the foot and toes, and the foot straightens and turns outwards as the toes push off. Overpronation occurs when the foot rolls inward too far. This causes all the muscles and tendons of the lower leg to twist excessively. Regular overpronation is believed to contribute to the development of many knee, lower leg and foot injuries such as heel spurs, plantar fasciitis, tendinitis and bunions. It is thought that as much as 60% of the population may overpronate.

Causes
You do not have to be a runner or athlete to suffer from overpronation. Flat feet can be inherited, and many people suffer from pain on a day-to-day basis. Flat feet can also be traumatic in nature and result from tendon damage over time. Wearing shoes that do not offer enough arch support can also contribute to overpronation.
Symptoms
Symptoms can manifest in many different ways. Here is a list of some of the common conditions associated with over-pronation in children. Achilles Pain. Ankle pain. Arch Pain. Low back pain. Heel Pain. Knee Pain (Runner's knee and Chondromalecia of the patella) Osgood Schlatter Disease (pain below the knee) Shin Splints (pain in the front of the lower leg) Over-pronation does not necessarily mean your child has "flat feet." Even though children's arches may be relatively high when they lie down or sit, over-pronation may not be seen until your child is standing. A certain amount of pronation is normal. During normal walking or running ("gait cycle"), the heel strikes the ground and the foot rolls inward to absorb shock and adapt to the surface. This gait cycle is even more important if the running surface is uneven.
Diagnosis
Your healthcare provider will ask about your symptoms, medical history, and activities and examine your feet. Your provider may watch you walk or run. Check the motion of your feet when they strike the ground. Look at your athletic shoes to see if they show an abnormal pattern of wear.
Non Surgical Treatment
Studies have shown that the most effective way to dexrease a high Q angle and lower the biomechanical stresses on the knee joint is to prevent excessive pronation with custom-maflexible orthotics. One study found that using soft corrective orthotics was more effective in reduknee pain than a traditional exercise program. A more recent study showed that Q angle asymmetries, secondary to excessive pronation affecting knee alignment, can be effectivecontrolled or corrected utilizing custom-made, flexible orthotics. Another project involving meof a running club determined that 75% of those using orthotics eliminated or greatly reduced pain in the feet, ankles, shins, knees and hips
Prevention
Many of the prevention methods for overpronation orthotics, for example, can be used interchangeably with treatment methods. If the overpronation is severe, you should seek medical attention from a podiatrist who can cast you for custom-made orthotics. Custom-made orthotics are more expensive, but they last longer and provide support, stability, and balance for the entire foot. You can also talk with a shoe specialist about running shoes that offer extra medial support and firm heel counters. Proper shoes can improve symptoms quickly and prevent them from recurring. Surgery can sometimes help cure and prevent this problem if you suffer from inherited or acquired pes planus deformity. Surgery typically involves stabilizing the bones to improve the foot?s support and function.
What Are The Causes Of Severs Disease?
Children with Sever's disease, which is also called calcaneal apophysitis, develop microfractures where the Achilles tendon inserts on the calcaneus, the large bone that makes up the heel of the foot. These microfractures cause pain, which can vary depending on the type of activity your child is doing, and is generally worse after activity and improves with rest. Sever's disease is more common in boys and typically occurs when a child is between 8 and 13 years old. Although it can affect both heels, it more commonly just affects one foot.
Causes
Mechanically, the heel takes a beating. And the apophyseal bone is located near the point of impact for the heel bone at heel strike and with most weight bearing activities. This includes running, jumping and walking. Heavy impact activities like soccer, football and gymnastics are commonly associated with this problem. In addition to this, there is traction on this apophyseal bone and the associated physeal line of growth cartilage. This traction on the apopysis (island of bone) along with the impact of weight bearing activities can lead to inflammation and pain. Tight Achilles and calf muscles also can contribute to this problem, and why stretching is discussed later.
Symptoms
The typical clinical presentation is an active child (aged 9-10 years) who complains of pain at the posterior heel that is made worse by sports, especially those involving running or jumping. The onset is usually gradual. Often, the pain has been relieved somewhat with rest and consequently has been patiently monitored by the patient, parents, coaches, trainers, and family physicians, in the expectation that it will resolve. When the pain continues to interfere with sports performance and then with daily activities, further consultation is sought. It should be kept in mind that failure to instruct patients and parents that continual pain, significant swelling or redness, and fever are not signs of Sever disease and therefore require further evaluation could result in failure to diagnose a condition with much more serious long-term consequences.
Diagnosis
Radiography. Most of the time radiographs are not helpful because the calcaneal apophysis is frequently fragmented and dense in normal children. But they can be used to exclude other traumas. Ultrasonography. could show the fragmentation of secondary nucleus of ossification of the calcaneus in severs?s disease. This is a safe diagnostic tool since there is no radiation. This diagnostic tool can also be used to exclude Achilles tendinitis and/or retrocalcaneal bursitis.
Non Surgical Treatment
Ice the heel(s) well after exercise (until the area is cold and numb!) Stretch hamstring and calf muscles 2-3 times daily (exercises below) REST when pain becomes persistent or moderate (even if it means skipping games or practices.) Anti-inflammatory medication such as ibuprofen. If symptoms persist, your child may need to see a physical therapist for additional exercises, and/or an orthopedist for othotics or temporary casting/crutches if pain is severe. Sever?s disease is self-recovering, meaning that it will go away on its own when the heels are rested or when the bone is through growing. The condition is not expected to create any long-term disability, and expected to subside in 2-8 weeks. However, pain can recur, for example at the start of a new sports season, several times if it is not taken care of.
Recovery
Recovery time will vary from patient to patient. Age, health, previous injuries, and severity of symptoms will affect recovery time. Your compliance with the stretching program and the other recommendations made by your doctor will also determine your healing time. Heel pain often completely resolves after a child?s heel bone has stopped its period of growth.
Flat Feet Symptoms
Overview
This condition is a progressive collapse of the tendons and ligaments that hold up the foot?s arch. This condition most commonly affects women. It typically occurs in only one foot, but in some cases, both feet are afflicted. 
Causes
Flat feet causes greater pressure on the posterior tibial tendon than normal. As the person with flat feet ages, the muscles, tendons and ligaments weaken. Blood supplies diminish as arteries narrow. These conditions are magnified for obese patients because of their increased weight and atherosclerosis. Finally, the tendon gives out or tears. Most of the time, this is a slow process. Once the posterior tibial tendon and ligaments stretch, body weight causes the bones of the arch to move out of position. The foot rotates inward (pronation), the heel bone is tilted to the inside, and the arch appears collapsed. In some cases, the deformity progresses until the foot dislocates outward from the ankle joint.
Symptoms
Symptoms are minor and may go unnoticed, Pain dominates, rather than deformity. Minor swelling may be visible along the course of the tendon. Pain and swelling along the course of the tendon. Visible decrease in arch height. Aduction of the forefoot on rearfoot. Subluxed tali and navicular joints. Deformation at this point is still flexible. Considerable deformity and weakness. Significant pain. Arthritic changes in the tarsal joints. Deformation at this point is rigid.
Diagnosis
In diagnosing flatfoot, the foot & Ankle surgeon examines the foot and observes how it looks when you stand and sit. Weight bearing x-rays are used to determine the severity of the disorder. Advanced imaging, such as magnetic resonance imaging (MRI) and computed tomography (CAT or CT) scans may be used to assess different ligaments, tendons and joint/cartilage damage. The foot & Ankle Institute has three extremity MRI?s on site at our Des Plaines, Highland Park, and Lincoln Park locations. These extremity MRI?s only take about 30 minutes for the study and only requires the patient put their foot into a painless machine avoiding the uncomfortable Claustrophobia that some MRI devices create.
Non surgical Treatment
Icing and anti-inflammatory medications can reduce inflammation and physical therapy can strengthen the tibial tendon. Orthotic inserts that go inside your shoes are a common way to treat and prevent flatfoot pain. Orthotics control the position of the foot and alleviate areas of pressure. In some cases immobilization in a cast or walking boot is necessary to relieve symptoms, and in severe cases surgery may be required to repair tendon damage. 
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Acquired Flat Foot Surgery
Overview Acquired adult flatfoot deformity (AAFD) is a progressive flattening of the arch of the foot that occurs as the posterior tibial tendon becomes insufficient. It has many other names such posterior tibial tendon dysfunction, posterior tibial tendon insufficiency and dorsolateral peritalar subluxation. This problem may progress from early stages with pain along the posterior tibial tendon to advanced deformity and arthritis throughout the hindfoot and ankle.  Causes The cause of posterior tibial tendon insufficiency is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot. Children nearly fully grown can end up with flat feet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs. Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur. Symptoms Patients will usually describe their initial symptoms as "ankle pain", as the PT Tendon becomes painful around the inside of the ankle joint. The pain will become more intense as the foot flattens out, due to the continued stretching and tearing of the PT Tendon. As the arches continue to fall, and pronation increases, the heel bone (Calcaneus) tilts into a position where it pinches against the ankle bone (Fibula), causing pain on both the inside and outside of the ankle. As the foot spends increased time in a flattened, or deformed position, Arthritis can begin to affect the joints of the foot, causing additional pain. Diagnosis The history and physical examination are probably the most important tools the physician uses to diagnose this problem. The wear pattern on your shoes can offer some helpful clues. Muscle testing helps identify any areas of weakness or muscle impairment. This should be done in both the weight bearing and nonweight bearing positions. A very effective test is the single heel raise. You will be asked to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the calcaneus (heel bone) in the middle with slight inversion (turned inward). X-rays are often used to study the position, shape, and alignment of the bones in the feet and ankles. Magnetic resonance (MR) imaging is the imaging modality of choice for evaluating the posterior tibial tendon and spring ligament complex. Non surgical Treatment Because of the progressive nature of PTTD, early treatment is critical. If treated soon enough, symptoms may resolve without the need for surgery and progression of the condition can be stopped. If left untreated, PTTD may create an extremely flat foot, painful arthritis in the foot and ankle, and will limit your ability to walk, run, and other activities. Your podiatrist may recommend one or more of these non-surgical treatments to manage your PTTD. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. Immobilization. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Physical therapy. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may recommend changes in your footwear.
Causes The cause of posterior tibial tendon insufficiency is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot. Children nearly fully grown can end up with flat feet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs. Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur. Symptoms Patients will usually describe their initial symptoms as "ankle pain", as the PT Tendon becomes painful around the inside of the ankle joint. The pain will become more intense as the foot flattens out, due to the continued stretching and tearing of the PT Tendon. As the arches continue to fall, and pronation increases, the heel bone (Calcaneus) tilts into a position where it pinches against the ankle bone (Fibula), causing pain on both the inside and outside of the ankle. As the foot spends increased time in a flattened, or deformed position, Arthritis can begin to affect the joints of the foot, causing additional pain. Diagnosis The history and physical examination are probably the most important tools the physician uses to diagnose this problem. The wear pattern on your shoes can offer some helpful clues. Muscle testing helps identify any areas of weakness or muscle impairment. This should be done in both the weight bearing and nonweight bearing positions. A very effective test is the single heel raise. You will be asked to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the calcaneus (heel bone) in the middle with slight inversion (turned inward). X-rays are often used to study the position, shape, and alignment of the bones in the feet and ankles. Magnetic resonance (MR) imaging is the imaging modality of choice for evaluating the posterior tibial tendon and spring ligament complex. Non surgical Treatment Because of the progressive nature of PTTD, early treatment is critical. If treated soon enough, symptoms may resolve without the need for surgery and progression of the condition can be stopped. If left untreated, PTTD may create an extremely flat foot, painful arthritis in the foot and ankle, and will limit your ability to walk, run, and other activities. Your podiatrist may recommend one or more of these non-surgical treatments to manage your PTTD. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. Immobilization. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Physical therapy. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may recommend changes in your footwear.  Surgical Treatment Surgery should only be done if the pain does not get better after a few months of conservative treatment. The type of surgery depends on the stage of the PTTD disease. It it also dictated by where tendonitis is located and how much the tendon is damaged. Surgical reconstruction can be extremely complex. Some of the common surgeries include. Tenosynovectomy, removing the inflamed tendon sheath around the PTT. Tendon Transfer, to augment the function of the diseased posterior tibial tendon with a neighbouring tendon. Calcaneo-osteotomy, sometimes the heel bone needs to be corrected to get a better heel bone alignment. Fusion of the Joints, if osteoarthritis of the foot has set in, fusion of the joints may be necessary.
Surgical Treatment Surgery should only be done if the pain does not get better after a few months of conservative treatment. The type of surgery depends on the stage of the PTTD disease. It it also dictated by where tendonitis is located and how much the tendon is damaged. Surgical reconstruction can be extremely complex. Some of the common surgeries include. Tenosynovectomy, removing the inflamed tendon sheath around the PTT. Tendon Transfer, to augment the function of the diseased posterior tibial tendon with a neighbouring tendon. Calcaneo-osteotomy, sometimes the heel bone needs to be corrected to get a better heel bone alignment. Fusion of the Joints, if osteoarthritis of the foot has set in, fusion of the joints may be necessary.